Introduction
Non-communicable diseases (NCDs) have emerged as a formidable global health challenge, with Sub-Saharan Africa (SSA) experiencing a significant and growing burden. In this context, cardiovascular diseases, cancers, diabetes, respiratory diseases, and stroke have become leading causes of ill-health, disability, and death, reflecting the combined impact of demographic shifts, epidemiological transitions, and the influences of modernization (WHO, 2015; Yiengprugsawan et al., 2016; Yiengprugsawan & Kendig, 2015).
Unique Challenges in Sub-Saharan Africa
Unlike the traditional perception of NCDs as diseases of affluence, NCDs are increasingly present across all contexts, including low- and middle resource areas. Moreover, SSA faces a distinctive set of challenges. The less readily acknowledged NCDs, including mental illnesses, dementia, and the long-term effects of accidents and injuries, contribute significantly to the overall burden. With nearly 41 million annual deaths, accounting for over 71% of global deaths, SSA experiences a severe “moral panic” and heightened pressure in public health settings (Subramanian et al., 2018; WHO, 2017, 2018b). This calls for urgent attention to address the nuanced dynamics of NCDs in the region.
Population Aging and Lifestyle Transitions
The increasing prevalence of NCDs in SSA is closely linked to population aging and evolving lifestyles. Older adults are undergoing a dietary transition, adopting an increasingly Westernized diet pattern and other health and social behaviors leading to rising rates of obesity and hypertension (Gyasi, 2018; Xu et al., 2016; Yiengprugsawan & Kendig, 2015). The correlation between NCD prevalence, aging, and key lifestyle risk factors such as tobacco use, physical inactivity, excess alcohol intake, and unhealthy diets underscores the need for targeted interventions (WHO, 2018a).
Economic Impact and Inequality
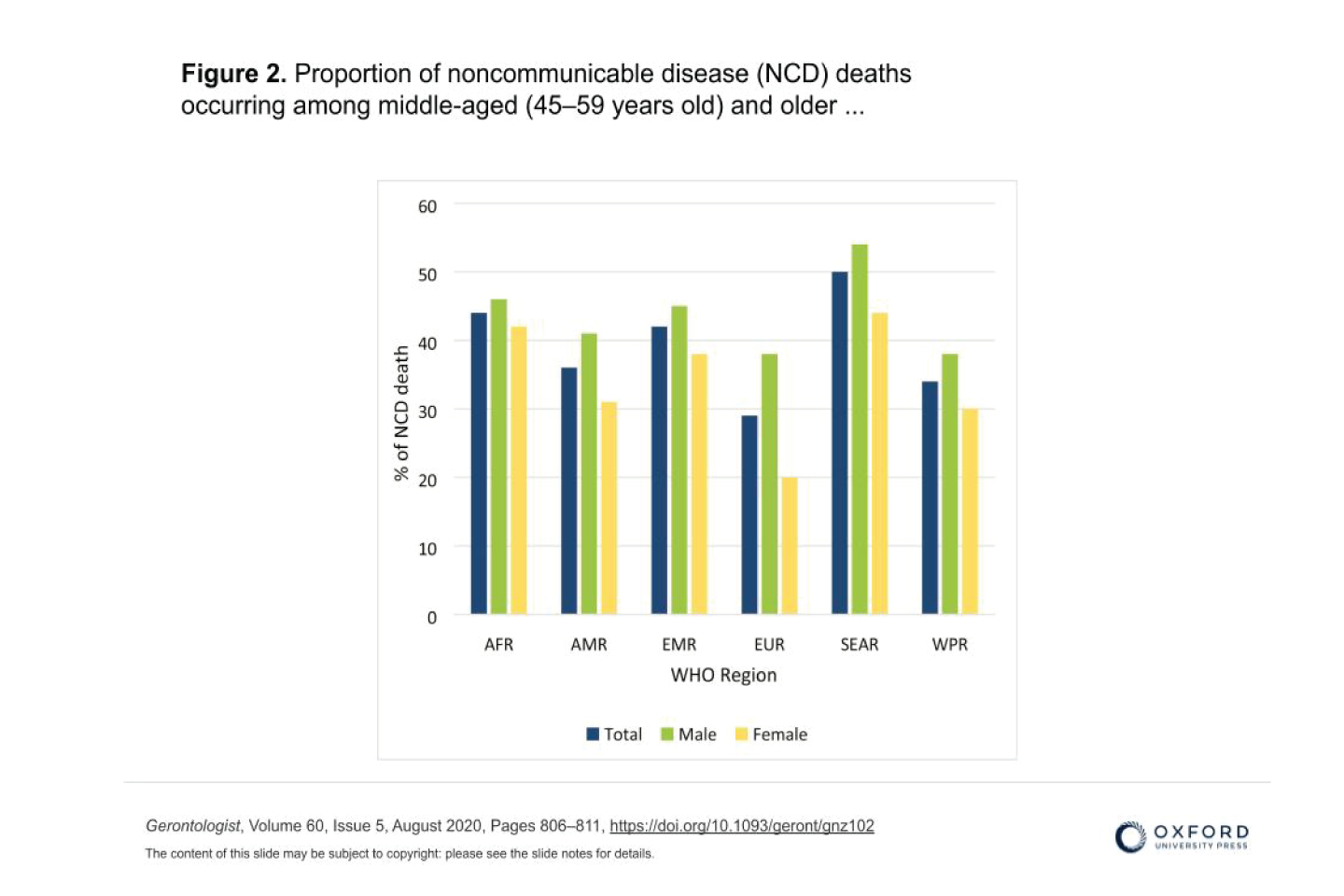
While economic impact data on NCDs are challenging to assess, projections indicate a doubling of the global economic burden from over US$6 trillion in 2010 to US$13 trillion by 2030. SSA, with more than 80% of all NCD-related deaths, faces a disproportionate share of this burden. The economic consequences of NCDs, including decreased productivity, premature deaths, and escalating healthcare costs, threaten to undermine the socioeconomic development of rapidly aging countries in SSA (Atun et al., 2013; WHO, 2014, 2018a).
Addressing Inequality and Implementing Preventive Measures:
The “double burden of disease” in SSA, encompassing both infectious conditions and NCDs, demands prioritized interventions. In a region where resource-poor and vulnerable groups bear a relatively greater burden, addressing the social gradient in health is crucial. Urgent regional and national action plans, akin to campaigns for infectious conditions, are essential. Furthermore, long-term care and NCDs in aging populations must receive attention, as indicated by the Western Pacific and African Regions of the WHO (WHO, 2017; WHO WPRO, 2017).
Policy Interventions and the Way Forward
To combat the rising prevalence of NCDs in SSA, comprehensive and locally tailored policies are imperative. The WHO Global Action Plan for the Prevention and Control of NCDs (2013–2020) recognizes the role of palliative care, a critical aspect often lacking in LMICs. National governments in SSA should prioritize access to palliative care services, effective self-management, and self-care practices, particularly for older adults.
Local solutions, supported by international bodies like the WHO, must be championed. Public education on NCD risk factors, culturally sensitive interventions, and promoting healthier lifestyles are key. Legislation to regulate and tax NCD-causing products can serve dual purposes of discouraging unhealthy habits and generating revenue for prevention and treatment campaigns.
Conclusion
In conclusion, the impact of NCDs in SSA presents a complex challenge rooted in poverty, malnutrition, poor sanitation, infections, and weak health and education systems. Regional and national efforts must focus on ensuring emotional and functional independence in old age, emphasizing the fight against NCD risk factors over the life course. As SSA undergoes rapid demographic aging, a life-course effort, engaging communities and families, becomes imperative to fully address the multifaceted challenges posed by NCDs in the region. The roles of culture, family structure, and social cohesion in providing social support for older people in SSA should be explored and exploited in future studies, making older persons the target of a comprehensive and engaged response to NCDs.